Ransome
’21, Art & Design
Painter and collage artist Ransome taps into his Southern roots and finds a creative community
Lesley students, alumni, faculty, and staff are making big things happen, from coast to coast and around the world.

Painter and collage artist Ransome taps into his Southern roots and finds a creative community

Saying ‘yes’ takes writer Faith Adiele on unforeseen journeys
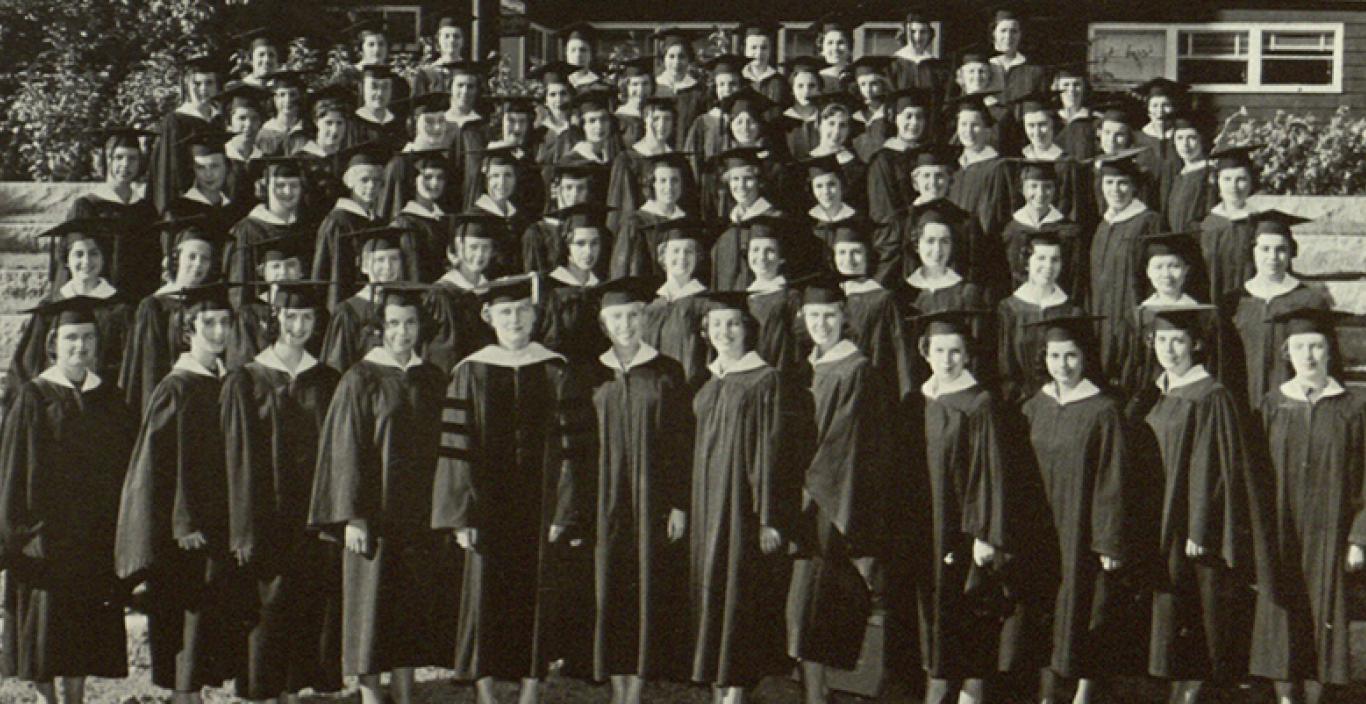
Classmates who first met in a freshman dorm in the fall of 1957 celebrate a milestone reunion and a lifetime of Lesley memories
Read more stories: Students | Alumni | Faculty & Staff